Plantar fasciitis is a common foot injury that affects the heel and is worsened by weight-bearing activity. Despite the name, plantar fasciitis is now called plantar fasciopathy because the mechanism is not caused by primary inflammation but rather by degeneration of the fascia (Rhim, et al., 2021). Plantar heel pain is another general term that describes plantar fasciopathy (Latt et al., 2020).
Both young and old, active and sedentary adults alike, are affected by plantar fasciopathy. Most of the time, there is not an acute event that leads to its onset but rather chronic weight-bearing activities and weakening of the foot and calf muscles, though some foot deformities do contribute (Boob, 2023).
This article will cover the most essential things personal trainers should know about plantar fasciopathy. Clients seeking training with heel pain are not uncommon, so it will be valuable for personal trainers to understand the structure and function of the plantar fascia, treatments, and exercise interventions that research has shown are effective.
Structure and Function of the Plantar Fascia
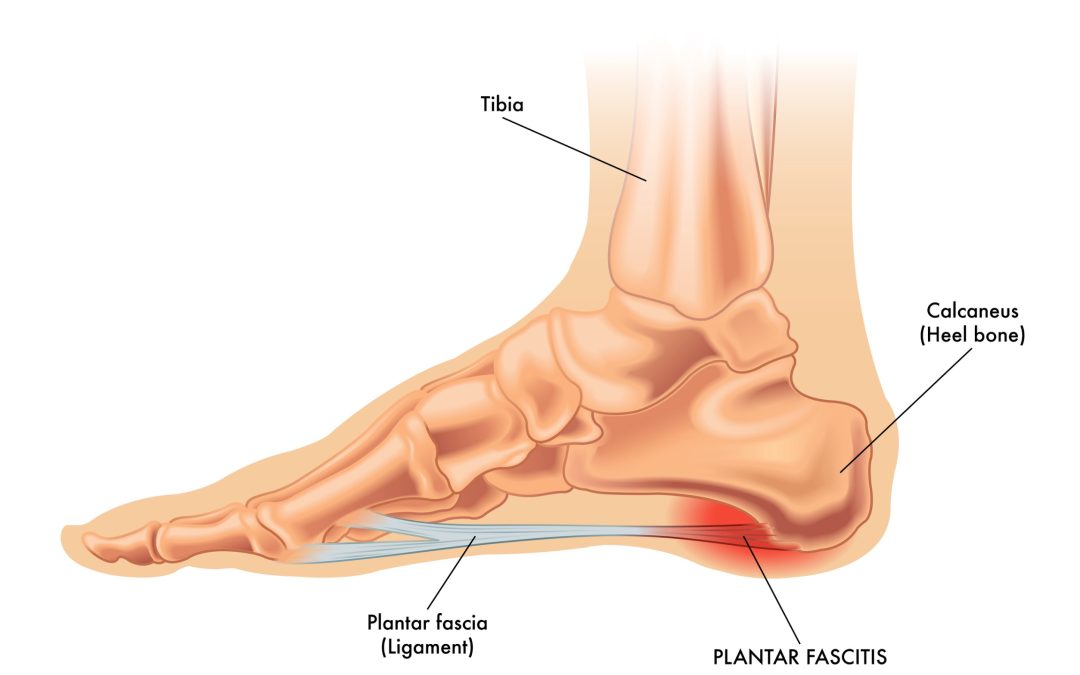
The plantar fascia comprises thick bands of fibrous and relatively inelastic connective tissue from the calcaneus to the proximal phalanges (Latt et al., 2020). It has three heads: the medial, lateral, and central bands.
The medial band inserts onto the muscles of the hallux, and the lateral band inserts on the base of the fifth metatarsal. The central band (the plantar aponeurosis) is the thickest, strongest, and most often involved in plantar fascia (Boob et al., 2023). It divides into five bundles at the midtarsal level, with each band attaching to one of the proximal phalanges, which, combined with the osseous structures of the arch, creates a rigid structure (Latt et al., 2020). 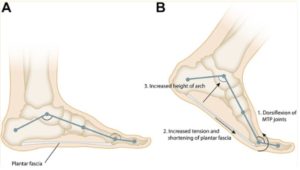
The plantar fascia stabilizes the arch during gait via the windlass mechanism. Dorsiflexion of the toes during terminal stance tightens the central band of the plantar fascia, pulling the metatarsal heads closer to the calcaneus and increasing the arch’s height (Latt et al., 2020). Inefficient foot function results in impairments of the gait cycle that create additional problems up the kinetic chain (Poenaru et al., 2021). 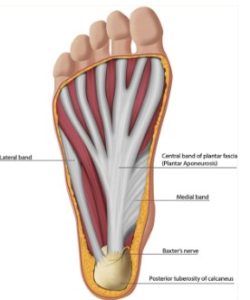
Poor foot posture exerts excessive stress on the muscles and joints of the lower limbs, which can cause anatomical changes across the body. If left untreated, it results in pain and dysfunction. When the foot’s dome is repeatedly exposed to impact loading, it flattens outward and diminishes stability in the region around the ankle joint (Poenaru et al., 2021). As a result of this instability and soreness, increased stress is transmitted via the knees, which display diminished joint space (Poenaru et al., 2021).
Epidemiology and Etiology
Plantar fasciopathy is responsible for over one million yearly doctor visits in the United States (Rhim et al., 2021). Pain may persist for over a year and be caused mainly by weight-bearing activities and after periods of inactivity. There are many medical causes of heel-related pain. Still, plantar fasciopathy is usually the culprit when severe pain is present in the morning, then gets better but worsens after continued weight-bearing activity (Latt et al., 2020).
Plantar fasciopathy usually starts from overuse or repetitive movement that causes micro tears rather than a sudden traumatic injury (Buchanan). This is why plantar fasciitis accounts for up to 22% of all running injuries and 83% of cases in active, working adults (Buchanan). The average age of those with it is between 25 and 65 years old, with women having a slightly higher incidence than men.
Risk Factors
The structural/physical risk factors for plantar fasciopathy include the following (Rhim et al., 2021):
- Pez planus occurs when the foot’s arch is flat, with weak foot muscles and low fascia tension.
- Pez cavus is when the arch of the foot is excessively high
- Limited dorsiflexion and tight gastrocnemius and soleus muscles, which often occur together.
- Excessive pronation and supination often occur with the risk factors mentioned above.
The risk factors above are crucial to recognize because they inherently affect the gait cycle and biomechanics, such as how weight is distributed on the foot when standing and walking (Latt et al., 2020). Obesity is also a strong risk factor because the heavier weight places more stress on the plantar fascia. Age and jobs requiring excessive standing are also strong risk factors.
Treatments
Surgical, therapeutic, and exercise treatments are primary treatment categories for plantar fasciopathy. The details of exercise treatment will be covered in the next section.
Surgery is used as a last resort after all other treatments have been exhausted without improvement. The first surgery option is called a plantar fasciotomy, which can be done endoscopically or open (Rhim et al., 2021). This involves a partial removal or cutting of the plantar fascia. Unfortunately, studies show that its effectiveness needs to be improved to warrant its use in most cases (Latt et al., 2020). The second type of surgery is less invasive and risky, in which the medial head of the gastrocnemius is partially cut, thereby lengthening the muscle, which should relieve tension on the plantar fascia.
Several treatments exist besides exercise or surgical intervention, including orthotic devices like arch supports and night splints, NSAIDs, corticosteroid injections, botulinum toxin, platelet-rich plasma, shockwave, ultrasound, acupuncture, and laser treatments (Boob et al., 2023; Poenaru et al., 2021). It is difficult to compare these treatments, but research shows that they can help reduce pain.
Some interesting findings were that custom orthotics were no better or worse at reducing pain and improving function than non-custom orthotics (Rhim et al., 2021; Latt et al., 2020). Also, pain relief from corticosteroid injections only lasts for one month (Rhim et al., 2021).
Exercise
Exercise is essential to improving plantar fasciopathy, especially with other treatments. It is also one of the most cost-effective treatments and provides countless health benefits. Some critical components of exercise techniques for plantar fasciopathy are strengthening, stretching, and foam rolling the foot and lower leg muscles. Reducing high-impact, repetitive movements in the lower leg is also critical to improving pain and function. Much research shows that these components effectively reduce pain (1-10).
As mentioned, foot and ankle instability, tight calves, reduced dorsiflexion, and toe extension are likely present in plantar fasciopathy. Therefore, exercises should be targeted to improve these dysfunctions. Remember, as personal trainers, we do not treat conditions but can provide exercises to enhance weak muscles, range of motion, etc.
An extended warm-up should be used for clients tolerating a typical workout with plantar pain. The warm-up should include all components of this exercise session, including lower leg stretching, foam rolling, and slow strengthening movements. Particular focus should be made on controlled and slow movements for strength training, focusing on the eccentric phase. Here are the main areas that you can work on with your client who has plantar fasciopathy:
Strengthening
Strength training is an effective strategy for improving the function of the lower leg and foot, which can improve symptoms (Lee et al., 2019; Riel et al., 2019). The most crucial factor in strength training is to use slow and controlled reps and avoid movements that provoke pain. Remember, the main variable to reduce is fast, explosive, and repetitive loading while exercising. Standard strength training recommendations can be followed.
- Strengthen the plantar and dorsi flexors through deficit training, such as from a wedge. These exercises include
- Calf raises
- Tibialis raises
- Sled pushing and pulling
- Heel elevated variations of lower body exercises
- Strengthen the plantar foot muscles by grabbing objects or scrunching up a towel with the toes
- Strengthen the ankle in the transverse plane of motion through eversion and inversion resistance exercises
Stretching
Remember that muscle strengthening in a full range of motion stretches the muscle. So, personal trainers should first help the client feel the stretch with every repetition of strength training. Perform a gastrocnemius, soleus, and plantar foot muscle stretch (Arif & Hafeez, 2022). Place a towel under the toes to extend the toes for a greater stretch.
- Remember to flex the knee and dorsi flex the ankle to stretch the soleus and extend the knee to target the gastrocnemius
- Hold stretches for 30 to 90 seconds at a time at a mild discomfort or moderate stretch perception unless pain is provoked.
- Stretch the calf multiple times (3+ sets) daily, especially in the morning and before activity or sedentary periods.
Self-myofascial release (SMR)
The central nervous system controls pain perception and the movement patterns associated with plantar fasciopathy (Sasun et al., 2024). Since neurological changes may contribute to symptoms, integrating neurological exercise techniques may improve symptoms (Sasun et al., 2024). The personal trainer can utilize SMR, proprioceptive neuromuscular facilitation, and two neurologically involved exercise techniques.
- Use tools such as foam rolling to improve outcomes (Ranbhor et al., 2021)
- Calf muscles
- Use of PNF in combination with SMR (find trigger point, hold pressure, and relax/contract muscle under pressure)
- Plantar surface muscles
- Use of PNF in combination with SMR (find trigger point, hold pressure, and relax/contract muscle under pressure)
Conclusion
In conclusion, personal trainers play a crucial role in supporting clients with plantar fasciopathy by understanding the structure and function of the plantar fascia and incorporating effective exercise strategies. By focusing on strengthening, stretching, and improving foot and ankle stability, trainers can help alleviate pain and improve function without stepping into medical treatment.
Slow, controlled strength exercises, alongside techniques like self-myofascial release and proprioceptive neuromuscular facilitation, are vital in addressing the muscular imbalances and dysfunctions associated with plantar fasciopathy. With these tools, personal trainers can enhance their clients’ quality of life and help them stay active despite heel pain.
Note: Images from: https://pubmed.ncbi.nlm.nih.gov/35097359/
References
- Arif MA, Hafeez S. Effectiveness of Gastrocnemius-Soleus Stretching Program as a Therapeutic Treatment of Plantar Fasciitis. Cureus. 2022 Feb 23;14(2):e22532. doi: 10.7759/cureus.22532. PMID: 35345689; PMCID: PMC8956500.
- Boob MA Jr, Phansopkar P, Somaiya KJ. Physiotherapeutic Interventions for Individuals Suffering From Plantar Fasciitis: A Systematic Review. Cureus. 2023 Jul
- Buchanan BK, Sina RE, Kushner D. Plantar Fasciitis. [Updated 2024 Jan 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: 31;15(7):e42740. doi: 10.7759/cureus.42740. PMID: 37654968; PMCID: PMC10467524.
- Gupta R, Malhotra A, Masih GD, Khanna T, Kaur H, Gupta P, Kashyap S. Comparing the Role of Different Treatment Modalities for Plantar Fasciitis: A Double Blind Randomized Controlled Trial. Indian J Orthop. 2020 Jan 20;54(1):31-37. doi: 10.1007/s43465-019-00038-w. PMID: 32257015; PMCID: PMC7093625.
- Latt LD, Jaffe DE, Tang Y, Taljanovic MS. Evaluation and Treatment of Chronic Plantar Fasciitis. Foot Ankle Orthop. 2020 Feb 13;5(1):2473011419896763. doi: 10.1177/2473011419896763. PMID: 35097359; PMCID: PMC8564931.
- Lee JH, Park JH, Jang WY. The effects of hip strengthening exercises in a patient with plantar fasciitis: A case report. Medicine (Baltimore). 2019 Jun;98(26):e16258. doi: 10.1097/MD.0000000000016258. PMID: 31261593; PMCID: PMC6617481.
- Poenaru D, Badoiu SC, Ionescu AM. Therapeutic considerations for patients with chronic plantar fasciitis (Review). Med Int (Lond). 2021 Jul 15;1(4):9. doi: 10.3892/mi.2021.9. PMID: 38939365; PMCID: PMC11208983.
- Ranbhor AR, Prabhakar AJ, Eapen C. Immediate effect of foam roller on pain and ankle range of motion in patients with plantar fasciitis: A randomized controlled trial. Hong Kong Physiother J. 2021 Jun;41(1):25-33. doi: 10.1142/S1013702521500025. Epub 2020 Oct 8. PMID: 34054254; PMCID: PMC8158403.
- Rhim HC, Kwon J, Park J, Borg-Stein J, Tenforde AS. A Systematic Review of Systematic Reviews on the Epidemiology, Evaluation, and Treatment of Plantar Fasciitis. Life (Basel). 2021 Nov 24;11(12):1287. doi: 10.3390/life11121287. PMID: 34947818; PMCID: PMC8705263.
- Riel H, Olesen JL, Jensen MB, Vicenzino B, Rathleff MS. Heavy-slow resistance training in addition to an ultrasound-guided corticosteroid injection for individuals with plantar fasciopathy: a feasibility study. Pilot Feasibility Stud. 2019 Aug 24;5:105. doi: 10.1186/s40814-019-0489-3. PMID: 31463078; PMCID: PMC6708237.
- Sasun AR, Babar T, Dadgal R. Effectiveness of Ankle Proprioceptive Neuromuscular Facilitation Techniques in Restoring the Biomechanical Integrity of the Ankle Following Plantar Fasciitis: An Experimental Study. Cureus. 2024 Jul 11;16(7):e64371. doi: 10.7759/cureus.64371. PMID: 39130914; PMCID: PMC11317122.
Brandon Hyatt, MS, CSCS, NFPT-CPT, NASM-CES, BRM, PPSC is an experienced leader, educator, and personal trainer with over 7 years of success in building high-performing fitness teams, facilities, and clients. He aspires to become a kinesiology professor while continuing to grow as a professional fitness writer and inspiring speaker, sharing his expertise and passion. He has a master's degree in kinesiology from Point Loma Nazarene University. His mission is to impact countless people by empowering and leading them in their fitness journey.