The effects of diabetes may be ameliorated by a well-designed exercise program, giving personal trainers an opportunity to do more for these clients than improving their fitness. By learning how to tailor programs to meet a diabetic’s needs, we can enhance quality of life and help effect changes in various health outcomes.
Diabetes is a disease that affects the body’s ability to produce or use insulin, the hormone responsible for transferring glucose from the blood to the cells. In the absence of insulin, or in cases of insulin resistance, excess sugar builds up in the bloodstream, setting off a cascade of potentially life-threatening situations.
The term Type 1 diabetes is used to describe a condition in which one’s pancreas does not produce any insulin at all. Type 2 diabetes occurs when insufficient insulin is released, or when one’s cells are insulin resistant and therefore unable to turn food into a necessary energy source.
Exercise is Key
Studies of individuals with Type 2 diabetes indicate that only about 38% participate in regular physical activity, compared with 58 % of healthy Americans. Sheri Colberg-Ochs, Ph.D., founder of the Diabetes Motion Academy in Santa Barbara, California and professor emerita of Exercise Science at Old Dominion University in Norfolk, VA underscores the impact of exercise on the diabetic patient: engaging in regular moderate exercise can help increase the body’s insulin action and keep blood sugar levels steady.
Type 2 diabetes responds to exercise on more than the level of blood glucose regulation: it can mitigate comorbid ailments often found in diabetic patients–cardiovascular conditions and obesity being the most profound. The potential to delay or even prevent the occurrence of Type 2 diabetes with exercise has been promoted by the medical community for decades. Regular workouts also afford the opportunity for improved balance among those diagnosed with Type 2 diabetes who are often considered “fall risks”.
Notably, exercise has also shown to help those with Type 1 diabetes lead healthier and more productive lives. For this patient, exercise increases insulin sensitivity, meaning less is required post-workout to process carbohydrates. Less insulin required equals fewer injections and improved functionality.
How Exercise Affects Diabetes
Moderate exercise causes an elevation in heart rate and respiration. Throughout this process, muscles utilize more of the glucose circulating in the bloodstream. Over time, this can lower blood sugar levels. With consistent workouts, the body’s response to insulin becomes more adept. Such benefits may last as long as 24 hours after a workout has been completed.
Two randomized trials each found that lifestyle interventions of ∼150 min/week of physical activity, when coupled with calorie counting and weight loss, lowered the risk of progression from glucose resistance to Type 2 diabetes by ~58%. In addition, a cluster-randomized trial found that diet alone, exercise alone, and a combination were equally effective in reducing this progression. Researchers hence conclude that increased physical activity and modest weight loss decrease the likelihood of increased diabetic conditions.
The Fitness Professional’s Role
Before engaging in a program of activity more vigorous than brisk walking, clients with diabetes should be carefully assessed by the personal trainer, keeping in mind that diabetics live with an increased likelihood of cardiovascular disease.
Careful exercise selection is key since a significant number of diabetics have a predisposition to injury. Ailments such as severe autonomic neuropathy, severe peripheral neuropathy, and proliferative retinopathy are a few of the more common roadblocks to progress. Learning the client’s age and physical activity history will help when designing a safe and effective training protocol.
It is important to inform clients that any variety of exercise is beneficial, but most individuals will stick with activities that they find enjoyable.
Here are a few suggestions to present to new or deconditioned diabetic clients:
- Walking, either outdoors or indoors on a track
- Participating in a dance class
- Cycling, outdoors or on a stationary bike
- Swimming/ water aerobics
- Stretch/balance classes
- Pilates, yoga or tai chi
- Tennis
- Aerobics/fitness class
- Engaging in household/ yard chores or gardening
- Resistance training with light weights or elastic bands
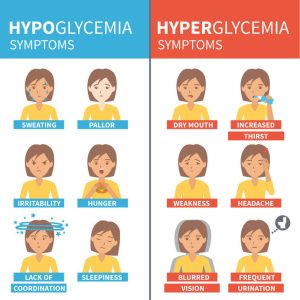
Dangers of Hyperglycemia
When individuals with Type 1 diabetes are deprived of sufficient insulin for 12–48 hours and have entered into a ketotic state, exercise can actually aggravate high blood sugar, or hyperglycemia. There is delicate balance to be monitored so it is important for the trainer to inquire about insulin injections before exercising.
Low insulin levels coupled with strenuous physical activity, promotes secretion of other hormones such as norepinephrine, epinephrine, glucagon and cortisol. Together, these substances cause the liver to release more glucose into the blood, thereby elevating blood sugar rather than promoting the desired lowering. This is particularly the case after an intense workout.
In the past, the American Diabetes Association had suggested that physical activity be avoided at fasting glucose levels >13.9 mmol/l (>250 mg/dl) and ketosis is present. Today, the position has been revised to state that, in the absence of very severe insulin deficiency, light- or moderate-intensity exercise still has the potential to decrease blood glucose.
It becomes the trainer’s job to ascertain whether the client feels well, is adequately hydrated, and is not showing overt signs of ketoacidosis:
- Excessive thirst
- Frequent urination
- Vomiting
- Weakness
- Shortness of breath
- Fruity-smelling breath
- Confusion
If the situation is deemed relatively safe enough for the client’s comfort level, it is not necessary to postpone exercise based solely on hyperglycemia.
Dangers of Hypoglycemia
The risk of potentially dangerous low blood sugar, or hypoglycemia, during or after exercise is elevated in the case of insulin deficiency. If a client is insulin-dependent, physical activity may lead to severe hypoglycemia if medication dosage or carbohydrate consumption is not altered in accordance with the intensity of exercise.
Type 2 diabetics run a slightly increased risk of developing hypoglycemia during or after exercise, although not to the extent of individuals reliant on insulin treatment. Since glucose is the body’s preferred energy source, a deficit of glucose renders the cells unable to function properly. For those diabetics on particular medications, even a short-term reduction in blood sugar can result in a cascade of complications. Blood sugar is considered low when it drops below 70 mg/dL. Immediate treatment for this situation will prevent more serious symptoms from developing.
Commonly exhibited symptoms of dangerously low blood sugar include the following:
- Blurry vision
- Rapid heartbeat
- Sudden mood changes
- Sudden nervousness
- Unexplained fatigue
- Pale skin
- Headache
- Hunger
- Shaking
- Dizziness
- Sweating
- Difficulty sleeping
- Skin tingling
- Trouble thinking clearly or concentrating
- Loss of consciousness, seizure, coma
Skipping meals, eating less than normal, or taking medication on time but eating a meal later than usual often lead to a precipitous drop in blood sugar levels. Something as simple as engaging in unplanned physical activity without sufficient nutrient consumption can also cause blood sugar levels to dip below an acceptable range.
Trainers might consider sending a text or email reminding a diabetic client to assess his blood sugar one to two hours before exercise, ensuring that it is within his normal target range at the time of training. If the level is below normal, consuming a small meal or snack rich in carbohydrates prior to the gym can be all that is necessary.
If a training session has been designed to extend for an hour or more, the consumption of additional carbohydrates during the workout can help thwart any problems. Exercise gels, sports drinks, fresh fruit or granola bars can provide a quick burst of necessary glucose during exercise. Remind the client to monitor his blood sugar immediately after exercise and every 2-4 hours afterward up until bedtime. For this reason, intense physical exercise immediately prior to retiring for the night is never recommended for diabetic clients.
Impact of Aerobic Exercise on Diabetes
Aerobic training increases insulin sensitivity, lung function, immune function, and cardiac output. Moderate to high volumes of aerobic activity are associated with lower cardiovascular risks in the healthy population, and the same holds true for those living with diabetes. Type 1 diabetics typically react to aerobic training with an increase in cardiorespiratory fitness, decreased insulin resistance, improvement in lipid levels, reduction A1C, triglycerides, and blood pressure.
Research published in Diabetes Care suggests that aerobic activity between 30 and 90 minutes has a positive effect on blood sugar, with more benefit seen with longer exercise sessions. Start out slowly for new or deconditioned clients, with an initial goal of 10-30 minutes of moderate physical activity, 5-7 days/week. As endurance builds, workouts may be extended incrementally.
Resistance Training and Reduction in Hypoglycemia
Diabetes is an independent risk factor for low muscular strength and an accelerated decline in muscle function. The health benefits of resistance training include improvements in muscle mass, body composition, strength, mental health, bone density, blood pressure and cardiovascular health. “If you lose muscle mass, you have a lot harder time maintaining your blood sugar,” Colberg-Ochs says.
While the effect of resistance exercise on glycemic control in Type 1 diabetes is not yet fully understood, it may assist in minimizing the risk of exercise-induced hypoglycemia. When designing workouts, starting with resistance exercises results in fewer reported episodes of hypoglycemia than when aerobic exercise is performed first.
Each session should include 5-10 different types of lifts involving the major muscle groups. For optimal strength gains, encourage the client to work up to 3-4 sets of 10-15 reps for each exercise. Programs for these clients may include weight training at least twice a week as part of their management plan — 3x is ideal, but always include a rest day between weight workouts. This is the time when they can engage in the other activities listed above.
Addressing Fall Risks
Similar to their healthy counterparts, flexibility and balance exercises are important for older adults with diabetes. Limited joint mobility is frequently present resulting in part from the normal aging process, but accelerated by hyperglycemia.
“I fully recommend that anyone over 40 with diabetes include balance training as part of their weekly routine, at least 2- 3 days/week,” says Dr. Colberg-Ochs. “It can be as simple as practicing balancing on one leg at a time, or more complex like tai chi exercises. Lower body and core resistance exercises also double as balance training.”
Balance training can reduce falls by 28%−29% as well as fostering improvements in gait, even when peripheral neuropathy is present. Stretching increases range of motion and flexibility around joints. Yoga has the potential of improving glycemic control, lipid levels, and body composition in clients with Type 2 diabetes. Tai chi training eases balance and neuropathic symptoms in adults with diabetes and neuropathy. Additional studies on this training would prove helpful.
Helpful Hints for Diabetic Clients
Regardless of the type of training planned for a personal training session, remind clients of the following:
- Wear well-fitting, comfortable shoes and cotton socks. Proper footwear can prevent blisters, which often lead to serious infections for many diabetics.
- Carry a snack or glucose tablets in case blood sugar bottoms out.
- Hydrate well before, during and after the workout.
- Always wear a diabetes ID necklace or bracelet while exercising.
While some of the challenges related to blood glucose management are universal in terms of the type of exercise involved, medication prescribed, and the presence/absence of diabetes-related comorbidity, many will vary from person to person. Thus, as with any of our clients, physical activity and exercise recommendations should be tailored to meet the specific needs of each individual.
Our goal is to help diabetic clients understand and incorporate moderate mindful movement into their daily lives, and develop strategies to avoid the potential complications of exercise. With the client’s permission, work with his medical team to determine the right program for his specific needs. Keep these professionals posted periodically on the patient’s workout progress and corresponding blood glucose levels.
References
https://www.everydayhealth.com/type-2-diabetes/living-with/great-exercises-for-people-with-diabetes/
https://www.verywellhealth.com/exercise-and-diabetes-how-much-is-enough-1086996
https://www.healthline.com/health/hypoglycemia
http://care.diabetesjournals.org/content/39/11/2065.abstract
http://care.diabetesjournals.org/content/11/2/201.short
http://care.diabetesjournals.org/content/29/6/1433.short
https://www.webmd.com/healthy-aging/features/exercise-lower-blood-sugar
Cathleen Kronemer is an NFPT CEC writer and a member of the NFPT Certification Council Board. Cathleen is an AFAA-Certified Group Exercise Instructor, NSCA-Certified Personal Trainer, ACE-Certified Health Coach, former competitive bodybuilder and freelance writer. She is employed at the Jewish Community Center in St. Louis, MO. Cathleen has been involved in the fitness industry for over three decades. Feel free to contact her at trainhard@kronemer.com. She welcomes your feedback and your comments!