It’s your job as an NFPT Trainer to help your clients reduce their lifestyle-related risk factors, which includes protecting bones and joints. Fit pros should be aware of, and situationally suggest fitness and wellness steps to reduce older clients’ risks for joint pains, poor posture, “inflammaging“, or (a subclinical inflammatory readiness, manifested by elevated levels of proinflammatory factors) and potential broken bones. Heightened awareness is key, as this public health message stated, “At least half of the age-related changes to muscles, bones, and joints are caused by disuse.”
A client’s bone density is only one skeletal issue for “PB&J.” Another issue is to help improve a client’s biomechanics to reduce lifestyle-related risk factors while encouraging her or him to use motion, rather than lapse into “disuse.” Even an elder sneeze can cause a bone break if porous bones are weak.
Key points addressed regarding protecting bones and joints:
- Four human tissue types (with a focus on our connective tissues as “Lean Mass”)
- Healthy vs. “Porous” Bones
- Connective Tissue matters
- Systematic steps to improve older clients’ activities of daily life with “PB&J.”
An ounce of prevention is truly worth many dollars of repair.
The National Osteoporosis Foundation now predicts that “porous bones” a.k.a. osteoporosis will lead to 3 million bone breaks at a total medical cost of $25 Billion USD annually. Once bones become abnormally porous, they are uncurable. Hence active and healthy lifestyles are superior to remedial and costly medical procedures. First, consider how human tissues support active and healthy lifestyles.
Four Human Tissue Types (Figure 1)
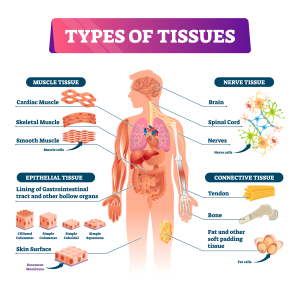
This comprehensive figure reinforces why humans are different than plants or inorganic things.
We have evolved to flee, fight, feed, and frolic. Both our lean mass and fat mass enable these four wellness functions. We have “honeycomb” bony skeletons to shield our organs and to provide joints against or across which muscles contract to create motion. When healthy, bones are completely “re-edited” via autophagy about every 10 years! So how do bones become unhealthy?
Bones may become weak, from one or many “nature and nurture” root causes, including:
- An inherited predisposition, e.g. parent(s) with hip fracture(s)
- Age for both genders and notably for post-menopausal women
- A low index “lean” body composition for bone, muscle, and water (!)
- Rheumatoid arthritis (RA)
- Smoking
- “Some” corticosteroids or other drugs use
- Excess alcohol intake, and
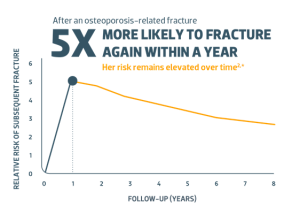
- Prior fracture(s) after age 50*
Note: For item 8:
* 
Healthy vs. Porous Bones
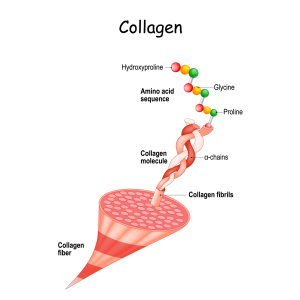
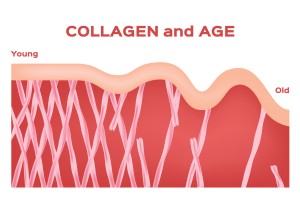
As critically important as are bones for motion/stability, red blood cell production, stem cell production, and storage of key micronutrients (magnesium, phosphorus, and calcium), they enable a fascinating network of biomechanical tissues, like fascia, as manifested by compounds like age-varying collagen (pictured here). In fact, collagen comprises the majority of our vital, bony “honeycombs”:
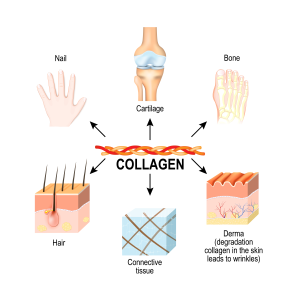
Connective Tissue Matters
As we age, our capacity to generate vital collagen (which is about 1/3rd of total body protein) diminishes greatly (see the right figure above). It is sad, but interesting that collagen loss happens at about the same rate as skeletal muscle loss (sarcopenia).
Collagen loss (and to lesser extent dehydration) is a reason for elder wrinkles, crepey-skin, and internal connective breakdowns that inevitably result from bodily senescence. A key connective tissue group, fascia, has predominant collagen in its composition. This sprinter in motion illustrates major fascia (IT bands, for example) that help us fight, flee or frolic:
 .Fascia can be considered a bodily “tablecloth” or a veneer that can cause bodily problems with injury, or “disuse.” One National Institute of Health article asserts,”Injuries to …fascial tissues cause a significant loss of performance in sports2 and have a potential role in the development and perpetuation of musculoskeletal disorders, including lower back pain.”
.Fascia can be considered a bodily “tablecloth” or a veneer that can cause bodily problems with injury, or “disuse.” One National Institute of Health article asserts,”Injuries to …fascial tissues cause a significant loss of performance in sports2 and have a potential role in the development and perpetuation of musculoskeletal disorders, including lower back pain.”
Self-myofascial release (SMR) is one approach to mitigate or prevent fascial injury (some of your clients may have experienced plantar fasciitis pains). Bespoken joint stretch routines are another.
How to Systematically Protect Bones and Joints
As this overview suggests, our bones and joints plus connective tissue are a networked, interconnected system. Thus, inter-connected advice and tailored regimens may be offered by Trainers. Why “tailored?” A client’s sore knee is different to address than overly tight IT bands, or plantar fasciitis pains.
Role of Diet
Trainers should be aware that supplements – such as bone broth – to possibly improve collagen levels are not principal solutions for decreased collagen levels. In half of our “osteo” deficiency cases, motion and use are principals.
We should be aware of “nutrients” and drugs that can accelerate the loss of collagen:
- Table Salt
- Soda
- Excess Caffeine
- Wheat Bran and
- Hydrogenated Oils (Poly-saturated or Trans-fat).
Imaging
Regarding bone mass, which comprises between 12-15% of body weight, peaks for both men and women at age ~40 and decreases steadily thereafter; elders and particularly women might be prescribed for imaging, either dual-energy X-ray absorptiometry (DXA) or Bioelectrical Impedance Analysis (BIA) methods (DXA or BIA).
Assess and Re-assess
Use your assessment skills to take note of your clients’ alignment. Is an elder’s noticeable shoulder tilt due to muscular weakness and/or possibly due to skeletal weakness or spinal osteoporosis? Awareness of past injury history, genetic predisposition, and other checklist items above will help us provide “low impact” exercises and lifestyle recommendations to avert many falls and fractures! Circling back to our introductory themes,
It is our job to provide appropriate fitness and wellness regimens to:
1. prevent lifestyle-related problems and
2. discourage client disuse, and encourage use in order to Protect Bones and Joints or “PB&J”.
Dave Frost has served the fitness community as a NFPT-certified CPT since 2013, and a Master Fitness Trainer since 2019.
As a Medicare-aged baby boomer, he specializes in training those clients who intend to stay “well past forty”.
He is a former world champion in Masters Rowing and National Indoor Rowing champion for his age group. He is also a group fitness instructor for The Row House. His website is https://wellpastforty.com. Dave recently published his work: KABOOMER: Thriving and Striving into your Nineties to promote stamininety for those intending to add years to their lives and life to their years.


