Why should trainers care about ankle dorsiflexion (DF)? After all – the DF muscles aren’t ones we often consider training much, if at all, and rarely ever discuss with our clients. You don’t see bodybuilders winning shows for their defined tibialis anterior, and most clients assume their lower leg muscles get “worked” enough with cardio exercises. This oft-neglected joint action is important to address because of its implication in larger movements.
Breaking Down Dorsiflexion
Ankle dorsiflexion occurs when you move your foot towards your leg in an open-chain activity, such as taking a step forward when walking. In a closed-chain activity, however, it allows the knees to translate anteriorly, as in descending into a squat.
[sc name=”anatomy” ]
Your knees translate forward in a variety of functional tasks and exercises, including lunges, step-ups, running, cutting, skipping, and more. Without proper ankle DF mobility, all these movements become impossible to perform with proper mechanics.
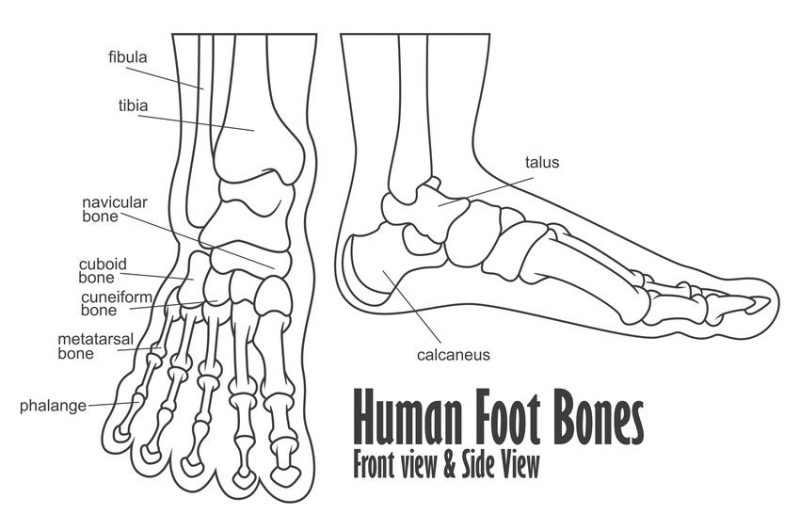
The anterior tibialis is the primary dorsiflexion muscle, however, optimal dorsiflexion involves some foot inversion as well, which means we have to look at the whole foot and ankle picture when assessing mobility and range of motion.
copyright: Rendix Alextian
Assessing DF
Optimal dorsiflexion for just walking is somewhere between 10 and 20 degrees. To descend into a squat without compensating, 35 degrees of dorsiflexion is needed.
One of the easiest ways to get a gross assessment of DF mobility is by using a goniometer, or by getting a goniometry app on your smartphone. Have your client assume a half-kneeling position and instruct them to bring their knee over their toes as far as they can while keeping their heel flat on the floor. Open a goniometer app on your phone, and place it on the client’s tibia. You now have a rough estimate in degrees of their closed-chain DF mobility, and if major imbalances exist between each side.
Compensations
Sure, someone may still be able to squat to parallel with limited ankle DF. But if you’ve lost mobility at the ankle and are still able to move the hips through a full range – something else is moving more than it should. Typically, this occurs at the foot, as we see compensatory subtalar joint pronation1 (1). That may not sound so bad until we remember that subtalar joint pronation causes tibial internal rotation and subsequently knee valgus collapse – the primary mechanism of injury for ACL tears and many other knee injuries (1, 2) at worst, and indicative of muscular imbalance at best.
The solution is to improve ankle DF mobility. Sure, we can start by releasing and stretching the calves, and strengthening the primary ankle DF muscles, such as the tibialis anterior. However, directly targeting the tibialis posterior will reap the greatest benefits in improving DF.
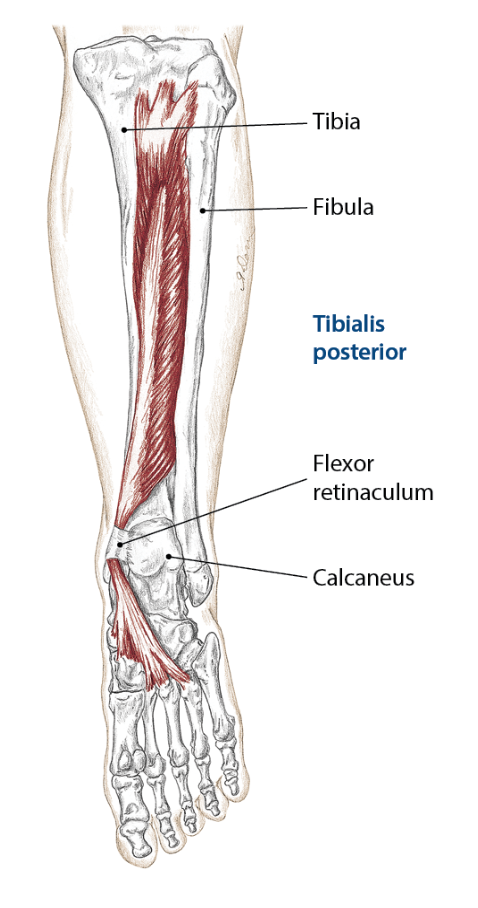
tibialis posterior, 2014 Books of Discovery
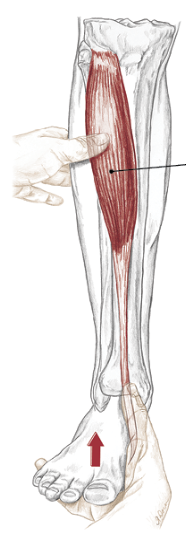
tibials anterior, 2014 Books of Discovery
The tibialis posterior is located deep to the gastrocnemius and soleus muscles, sandwiched between the flexor digitorum and hallucis longus and attaches to the back of the tibia as its name suggests. It runs from the proximal posterolateral tibia, posteromedial fibula and interosseus membrane to the navicular bone in the foot. Important enough to note: this muscle stabilizes the medial arch of the foot. Although it assists in plantarflexion, it is also a primary mover of ankle inversion (3).
This ankle inversion piece is our primary focus in closed chain ankle motion at the subtalar joint in the foot. For the talus to dorsiflex within the mortise of the ankle joint formed by the tibia and fibula, the calcaneus (aka, subtalar joint) must invert (4).
Strengthening Dorsiflexion
We’ve identified our key player, but how do we strengthen this specific muscle without strengthening the gastrocnemius and soleus (which we are trying to stretch, remember)?
EMG research has shown the tibialis posterior exhibits increased activity in a position of 30-degrees of adduction (5). Since this muscle is closely linked with adduction, a ball-squeeze calf raise can also be used which, if the great toes of each foot are touching, will place the talus in adduction while also strengthening inversion. As you know, training must match specific goals, and strengthening the tibialis posterior muscle in a foot-forward position by keeping the great toes apart and feet neutral as is seen in various exercises and running will result in the best carryover.
[sc name=”anatomy” ]
 Dan Braun is an NFPT-CPT and 2020 graduate of Lebanon Valley College’s Exercise Science program. Braun is currently enrolled in LVC’s Doctor of Physical Therapy program and will graduate with his DPT in 2022. While in school, Dan runs his own training business and podcast (Brawn Body Health and Fitness Podcast, available on all major streaming platforms).
Dan Braun is an NFPT-CPT and 2020 graduate of Lebanon Valley College’s Exercise Science program. Braun is currently enrolled in LVC’s Doctor of Physical Therapy program and will graduate with his DPT in 2022. While in school, Dan runs his own training business and podcast (Brawn Body Health and Fitness Podcast, available on all major streaming platforms).
References:
- Bell, D. R., Oates, D. C., Clark, M. A., & Padua, D. A. (2013). Two- and 3-dimensional knee valgus are reduced after an exercise intervention in young adults with demonstrable valgus during squatting. Journal of athletic training, 48(4), 442–449. https://doi.org/10.4085/1062-6050-48.3.16
- Shimokochi, Y., & Shultz, S. J. (2008). Mechanisms of noncontact anterior cruciate ligament injury. Journal of athletic training, 43(4), 396–408. https://doi.org/10.4085/1062-6050-43.4.396
- Drake RL, Vogl W, Mitchell AWM. Gray’s Anatomy for Students. 2nd Ed. Philadelphia: Churchill Livingstone Elsevier, 2010.
- Levangie, P. K., & Norkin, C. C. (2005). Joint structure and function: a comprehensive analysis. 4th ed. Philadelphia, PA: F.A. Davis Co.
- Akuzawa, H., Imai, A., Iizuka, S., Matsunaga, N., & Kaneoka, K. (2017). The influence of foot position on lower leg muscle activity during a heel raise exercise measured with fine-wire and surface EMG. Physical therapy in sport: official journal of the Association of Chartered Physiotherapists in Sports Medicine, 28, 23–28. https://doi.org/10.1016/j.ptsp.2017.08.077
Guest authors offer experience and educational insights based on their specific area of expertise. These authors are contributing writers for the NFPT blog because they have valuable information to share with NFPT-CPTs and the fitness community at-large. If you are interested in contributing to the NFPT blog as a guest, please send us a note expressing your interest and tell us how you can contribute valuable insights to our readers. We look forward to hearing from you! Send to editor@nfpt.com

