Personal training clients may, from time to time, report some degree of cartilage damage or injury, frequently caused by overzealous participation in sports-related endeavors. Fortunately, there are various approaches to fostering new cartilage growth, and may prove to be bona fide game-changers in terms of restoring joint health.
Tissue Damage and Injury
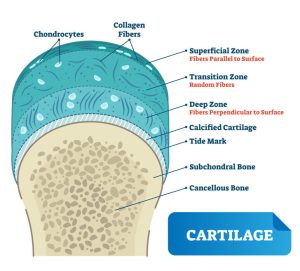
Cartilage, the tough yet flexible connective tissue covering the surface of joints, acts as the shock absorber between bones. Whether through the ravages of repetitive motions, osteoarthritis, frequent sports injuries, or simple wear-and-tear, cartilage damage ranks as a primary cause of knee/hip/ankle problems. While many such injuries can typically heal within a few weeks’ time given appropriate rest and rehabilitation exercises, more severe cases may require invasive procedures or surgical repairs.
Cartilage Damage Symptoms and Treatments
Symptoms of cartilage damage bear a striking resemblance to those of sprains ~
- Pain that continues even when resting
- Swelling
- Stiffness
- Inability to bear weight
- “clicking”, locking and/or giving way of the joint
Only a professional can accurately diagnose the source/severity of joint pain. If damage does not respond to less invasive treatments, surgical options exist that can offer positive outcomes.
Copyright: <a href=’https://www.123rf.com/profile_normaals’>normaals</a>
Rebuilding the Foundation
In addition to the all-too-common joint replacement operations, some new and innovative treatments have met with great success, most notably the potential of cartilage to repair itself. While much more research will help elucidate this process, scientists at Duke Health Center have found similarities to the manner in which salamanders and zebrafish regenerate limbs. This looks promising as a potential osteoarthritis treatment.
According to Virginia Byers Kraus, M.D., Ph.D., Professor of Medicine, Pathology and Orthopedic Surgery at Duke, “We believe that an understanding of this ‘salamander-like’ regenerative capacity in humans, and the critically missing components of this regulatory circuit, could provide the foundation for new approaches to repair joint tissues and possibly whole human limbs.”
Drilling For Growth
Microfracture, a fairly new procedure, attempts to stimulate the growth of new cartilage by creating a fresh blood supply.
This surgical procedure utilizes a sharp tool to create multiple holes in the subchondral bone, the layer just under the cartilage. This process encourages a healing response by allowing blood to reach the surface of the joint. In theory, the newly emergent cells will form cartilage. To date, this procedure has seen great success.
Stem Cells Driven to Create Cartilage
In the field of tissue engineering, scientists attempt to isolate human growth factors to induce new cartilage formation. Mesenchymal stem cells obtained from healthy bone marrow have demonstrated the ability to yield cells similar to the host tissue when cultured in the proper environment. While this field still qualifies as “experimental”, researchers hope to show how stem cells placed near a damaged joint surface may over time stimulate hyaline cartilage growth.
During the developmental stages of maturing bone, cells must first enter a cartilage-forming phase. Medical professionals propose halting bone-forming evolution at the point where cells begin forming cartilage utilizing a molecule known as VEGF (vascular endothelial growth factor). VEGF works by blocking further signaling molecules from completing the process.
The result of one such attempt yielded cartilage comprised of the same sort of cells as natural cartilage, with comparable mechanical properties. Even human tissue embedded into mice proved capable of driving bone growth, engineered to stop precisely at the stage of cartilage development.
Membrane-Induced Autologous Chondrocyte Implantation (MACI)
MACI, another fairly new surgical procedure, utilizes cartilage-forming cells, or chondrocytes, obtained from one’s own body to help restore damaged cartilage in other joints. Once harvested through needle biopsy aspiration, chondrocytes can then multiply in a laboratory setting. Upon reaching a sufficient quantity, surgeons can implant the cells into a damaged joint area, where they will continue to proliferate.
[sc name=”functional” ]
Platelet-Rich Plasma Therapy (PRP)
Platelet-rich plasma refers to a volume of autologous plasma replete with a platelet concentration well above baseline. Normal platelet counts average about 200,000/1J.1; a mere 5 ml. of plasma containing PRP with 1,000,000 platelets/1J.1 seems to show success at enhancing the healing of both bone and soft tissue.
Platelet-rich plasma contains an abundance of growth factors – seven in all — in their naturally occurring biological ratios, typically utilizing a clot as the carrier. However, PRP alone cannot induce new bone formation. Only bone morphogenetic proteins (BMPs) harbor this ability. With further study, scientists hope to demonstrate how PRP may accelerate the traditionally slow BMP activity.
PRP, Osteoarthritis, and Healing
A variety of factors can affect the progression of osteoarthritis (OA), including inhibition of inflammatory cytokines to ameliorate enzymatic expression. PRP therapy aims at mediating inflammation and catabolism through the secretion of anti-inflammatory factors. Many recent studies have demonstrated the clinical benefits of PRP in the non-operative management of OA. The future of PRP and its application for cartilage repair/regeneration looks promising, as scientists seek to focus on customization/tailoring of biological factors by targeting disease-specific markers.
A February 2021 study from the Department of General Surgery and Medical-Surgical Specialties, Orthopedics and Traumatology at the University of Catania, Italy yielded the following results:
“PRP supplies and releases cytokines, growth factors, and α-granules, all of which can offer a recovering stimulus and promote healing and tissue repair. The PRP injection can promote the release of fibrinogen, a substance that helps in wound healing or a ligament tear, interleukin-1 receptor antagonist as an anti-inflammatory, tissue growth factors, platelet-derived growth factors and vascular endothelial growth factors.”
Each of these growth factors stops an overactive inflammatory response from degrading tissue, and modulates angiogenesis (the development of new blood vessels to facilitate healing). The use of PRP directly at the site of cartilage injury most likely can stimulate natural healing by accelerating the cultivation of new tissue.
Additional Approaches
Supplementation, from vitamins to protein, remains a popular yet controversial route. Over-the-counter natural substances such as shark fin cartilage, glucosamine chondroitin, and MSM have enjoyed a high level of popularity, mostly through anecdotal evidence. Whether these products show any benefit when compared to growth of fresh cartilage cells remains uncertain, since strong evidence appears on both sides. We encourage personal trainers — and all readers — to continue seeking out innovative research data on this topic before making any recommendations to clients.
References:
https://pubmed.ncbi.nlm.nih.gov/24212369/
https://pubmed.ncbi.nlm.nih.gov/25068847/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6220001/
https://www.webmd.com/fitness-exercise/platelet-rich-plasma-injections#1
https://www.cartilageregenerationcenter.com/shoulder
https://bionumbers.hms.harvard.edu/files/recensioneprp1.pdf
https://www.hopkinsmedicine.org/orthopaedic-surgery/specialty-areas/sports-medicine/cartilage-regeneration.html
https://med.stanford.edu/news/all-news/2020/08/Researchers-find-method-to-regrow-cartilage-in-the-joints.html
https://orthoinfo.aaos.org/en/treatment/articular-cartilage-restoration
https://advances.sciencemag.org/content/5/10/eaax3203
https://healthcare-in-europe.com/en/news/regrow-cartilage-in-joints-science-says-you-can.html
https://www.nhs.uk/conditions/cartilage-damage/
Cathleen Kronemer is an NFPT CEC writer and a member of the NFPT Certification Council Board. Cathleen is an AFAA-Certified Group Exercise Instructor, NSCA-Certified Personal Trainer, ACE-Certified Health Coach, former competitive bodybuilder and freelance writer. She is employed at the Jewish Community Center in St. Louis, MO. Cathleen has been involved in the fitness industry for over three decades. Feel free to contact her at trainhard@kronemer.com. She welcomes your feedback and your comments!

