Knee pain and complaints are common among personal training clients. A clear understanding of the internal knee and knee function supports knowledge to program restorative knee exercises, progressions, and regressions.
Knee Anatomy
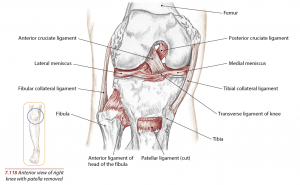
The knee is the junction of the femur, tibia, fibula, and patella bones. Ligaments, tendons, fascia, and muscles connect the joint and allow movement.
Technically named a synovial joint, the knee is more specifically referred to as a “hinge” joint for its linear and door-like movement patterns. When the knee is flexed it can, in fact, perform internal and external rotation!
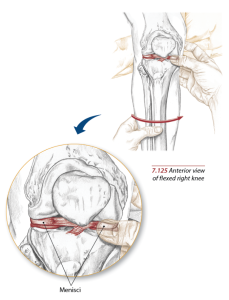
The knee joint has four ligaments along with the menisci, a type of hybrid cartilage/ligament that acts as a shock-absorbing barrier between the articular cartilage on the ends of the femur and tibia.
Lateral Collateral Ligament (LCL)
The LCL is also called the “fibular collateral ligament” because it connects the lateral femur and fibula. LCL limits the sideways motion of the knee. Any hyper or excessive movement in which the knee has to over stabilize against a sudden change of direction that the surrounding musculature can’t control could damage this ligament.
Medial Collateral Ligament (MCL)
The MCL is also called the “tibular collateral ligament” because its attachment sites connect the medial femur and tibia. Like the LCL, the MCL limits the sideways motion of the knee and is generally injured when the stress of quickly changing directions overpowers the force and stabilizing abilities of the surrounding musculature.
LCL and MCL Causes of Injury
Anytime the knee is subject to sideways motion the LCL and MCL are prone to injury. Sports like racquetball, tennis, basketball, football, and soccer are places for potential injury. Also, stepping out of a car, bumping a corner in a grocery store aisle, or missing a step while walking can place lateral-medial stress on the knee.
MCL Sprain or Tear
MCL injuries occur when the knee is struck on the lateral part (Outside) of the body. Since the MCL is located in the inside part (Medial) of the knee and resists widening of the inside of the knee joint when the knee is struck from the outside with a force that causes lateral buckling it simultaneously separates and widens the medial portion of the knee joint causing the injury.
MCL tears are classified by their severity into three categories.
- Grade 1– This is an incomplete tear of the MCL. The tendon is still in continuity and there are minimal symptoms. The symptoms are pain on the MCL with minimal downtime where most can return to their normal activities or sports within a few weeks’ time
- Grade 2– A grade two tear is also an incomplete tear but with more aggravated symptoms such as more intense swelling and pain along with a feeling of instability. A period of at least three to four weeks of rest is usually necessary.
- Grade 3– This is a complete tear of the MCL. There is significant swelling and pain with difficulty bending the knee. Instability or the knee giving out are common findings. A period of at least six weeks or longer is needed for healing to occur. Having a knee brace with lateral and medial stabilizers is recommended. Due to the good blood supply that the MCL has and usually responds well to non-surgical treatments, it is rarely treated with surgery.
LCL Sprain or Tear
LCL injuries are the complete opposite of MCL tears. They occur when the inside (medial part) of the knee is struck and pushed out or in sports where there are a lot of quick stops and turns as in soccer, basketball, and skiing. LCL injuries are also classified by their severity with classifications and symptoms similar to those of the MCL. However, the LCL does not heal as well as the MCL and in most cases, a Grade 3 injury will require surgery.
2014 Books of Discovery
Anterior Cruciate Ligament (ACL)
The word “cruciate” means crossing from one side to the other and/or one over the other. The ACL connects the femur to the tibia along the front center part of the knee. Specifically, one end connects to the anterior tibia along the medial side of the tibias’ sagittal line.
The other end connects to the deep portion (almost to the rear but not quite) of the femur along the lateral side of the femur’s sagittal line. If you look carefully you can identify a slight diagonal angle to this ligament.
The ACL, one of the most common ligaments injured in sports, is responsible for controlling the allowable rotation of the knee along with limiting the forward trajection of the tibia under the femur during, but not limited to, squatting, lunging, landing, running, and walking.
The ACL is most commonly injured by quick rotational movements where the foot is planted but the upper body is changing directions in a rotational fashion. Imagine a basketball player coming down from a rebound and accelerating with the upper torso in a direction opposite to how the feet are grounded without pivoting. Ouch!
Posterior Cruciate Ligament (PCL)
The PCL is the strongest ligament and primary stabilizer of the knee, also connecting the femur to the tibia but through the posterior side. The PCL limits the backward motion of the knee and may also prevent medial-lateral (side-to-side) and rotary movements.
Another injury-prone example would be someone washing dishes with both feet grounded and abruptly twisting the upper torso, hips, and femur in directions opposite to those in which the feet are facing without allowing for a slight pivot or complete re-positioning of the foot.
ACL Sprain or Tear
An ACL tear is most often a sports-related injury but can also occur during rough play, auto accidents, falls, and work-related injuries. Most ACL injuries in sports happen when pivoting or landing from a jump. Similar to meniscus injuries, patients with ACL tears often feel a “pop” and the knee usually gives out underneath them.
Subsequent pain and swelling is to be expected. ACL tears do not necessarily require surgery. According to Doctor Jonathan Cluett, Board-Certified Orthopedic Surgeon in Massachusetts, your daily activities and demands should be considered prior to opting for surgery.
For instance, do you regularly perform activities such as football, soccer, basketball, skiing, gymnastics, hockey, wrestling, lacrosse, rugby, singles tennis or cheerleading that require a normally functioning ACL? Secondly, is your knee stable? If not, you may not need ACL surgery. Many patients with ACL injuries feel better within a few weeks. The only persistent problem may be instability.
PCL Sprain or Tear
PCL injuries are most commonly experienced when the knee is bent and an object forcefully strikes the shin backwards. This type of injury can be experienced in a car collision when the shin strikes the dashboard. The other mechanism of injuring the PCL is in sports when an athlete falls on the front of the knee.
The knee is hyperflexed with the foot held in a pointing downwards position. Symptoms of PCL injuries are quite similar to those of ACL injuries. In the weeks following the injury patients state that they can’t trust their knee or that it feels as it is going to give out.
Knee Cartilage
Cartilage, sometimes referred to as “articular cartilage”, can be found at the end of the fibula, tibia, fibula, and behind the patella. Cartilage is a type of connective tissue that has no blood vessels or lymphatics, which makes it a type of tissue that is very slow to heal. It also has no nerves and is therefore insensitive.
A major function of cartilage is to absorb impact, especially in the knees, and transfer forces in a pain-free manner.
2014 Books of Discovery
In the knee, there are two types of cartilage:
- Hyaline – which covers the end of the femur, tibia, and fibula.
- Menisci – a specialized hybrid type of cartilage that provides for the needed cushioning between the femur and tibia. Learn about meniscus anatomy and injuries in this article.
Composition of Knee Ligaments & Cartilage Structures
Ligaments, which connect one bone to another, are composed of approximately 70% water and 30% organic matrix along with fibrocytes, the specific type of cells that make up tendons and ligaments.1,2
The organic matrix is a combination of ground substance (a combination of protein and carbohydrate complexes forming a gel-like substance) and collagen. In ligaments and tendons, 90% of the Organic Substance is collagen.
Collagen comprises 25 to 30% of the protein in the body with at least 15 types of collagens currently known with more recent studies identifying more than 20 types!2,4 Collagen production in the body can vary from individual to individual with the aging process and genetics playing the biggest role in the ability to make adequate amounts for tissue repair and maintenance.
In tendons and ligaments, the type of collagen found is called Type 1, which identifies its structural alignment, splice variants, and function when compared to the other many types of collagen in the body. 3, 4
Type 1 collagen fibers tend to be more rigid than Type 2. Hence, the ability to withstand the forces generated by movement and keep the bones they hold together without a daily injury. Cartilage, which covers the end of all bones that touch each other, is a bit different in its composition when compared to ligaments and tendons.
When discussing the ligaments above and as will be discussed in part 2 of this series when we cover tendons, the cells that make up those structures are called “fibrocytes”. In cartilage, the cells are called chondrocytes and the type of collagen is Type 2 as compared with Type 1 in tendons and ligaments.1,6,7
Varieties of Cartilage
In the human body, we can find three (3) types of cartilage:
- Hyaline or articular cartilage is found at the end of long bones in the body. It is bluish-white in color, flexible, with low friction qualities that resist wear and tear and designed to bear and distribute loads. Hyaline cartilage provides the cushioning needed for repetitive movements.
- Fibrocartilage is present in the intervertebral disks of the spine, covering the mandibular condyle in the temporomandibular joint, and in the Meniscus of the knee. It is also found temporarily at bone fracture sites.
- Elastic cartilage is found in the pharyngotympanic tubes, epiglottis, and earlobes where the supportive tissue (cartilage) must possess elasticity (hence, the name “elastic” cartilage).
Chondromalacia Patella
Chondromalacia Patella is the degeneration of the cartilage between your patella and femur. Your kneecap, which sits over the front of the knee joint, glides over the Femur as your knee bends or extends. Chondromalacia Patella (also called “Patellofemoral Syndrome”, “Runners Knee”, “Patellar Tendinitis” or “Jumpers Knee”) begins when the kneecap does not move properly and rubs against the lower part of the femur.
Causes of chrondomalacia patella:
- The kneecap is in an abnormal position(also called poor alignment of the Patellofemoral joint)
- Tightness or weakness of the muscles on the front or back of the thigh
- Flat feet
- Too much physical activity that places extra stress on the kneecap
Symptoms of Chondromalacia Patella are pain behind, below or on the sides of the kneecap being more noticeable while climbing up or down stairs, performing deep knee bends, standing for long periods and running downhill.
Prepatellar Bursitis
Prepatellar Bursitis is the common cause of swelling and pain on top of the kneecap. The bursa are thin sacks filled with the body’s own natural lubricating fluid. The bursa are very thin slippery sacks that are situated around our joints to prevent muscles, tendons and skin from catching on bony surfaces throughout the body.
When there is trauma, repetitive use or injuries to the knee, the bursa can swell and either fill up with blood or fluid, which in turn causes pain and swelling of the knee. If the trauma is associated with a tear in the skin the bursa can become infected, this is called infected bursitis.
Kneeling daily for extended periods of time or being sedentary increase the risk for prepatellar bursitis.
Symptoms of prepatellar bursitis are:
- Swelling over the kneecap
- Limited motion of the knee
- Painful movement of the knee
Bursitis of the knee can be treated by draining the bursa sac and in cases where infection is possible, an antibiotic is prescribed. In mild cases, resting the site along with ice therapy and anti-inflammatory medication may work just fine.
How Personal Trainers Can Program For Knee Pain
Personal trainers aren’t allowed to directly treat pain, but you can strengthen the muscles supporting the joint to hopefully alleviate it as an outcome.
Non-injury-related knee pain is a common issue trainers come across. Like most chronic joint pain, it is often due to overuse, misalignment, or muscular strength imbalances. Knees are quite susceptible to these causes, considering the overwhelming prevalence of bad posture, sitting most of the day, and weekend warriors.
Don’t misunderstand, I do not find it “wrong” to only workout here and there when time allows. However, it is the sporadic participation in high-intensity activity common with weekend warriors that can put the body at risk for pain or injury. When one is not necessarily accustomed to regular exercise, misalignment, and improper body mechanics can be a result.
Running, biking and other extreme sports clients may not have had an actual injury, but their knees are likely tired and may not have been properly cared for.
Why Do Knees Cause Problems?
One of the common reasons for knee pain and injury is improper tracking of the kneecap. The hip joints are wider than the knee joints in a neutral standing position. Unfortunately, the natural human anatomy promotes an uneven contraction of the quadriceps.
The effect is that when the knees are straightened the kneecaps are slightly pulled in a lateral direction. The vastus medialis is responsible for correcting this lateral diversion, and is also one of the most neglected muscles of the quadriceps group.
It tends to be the outer thigh muscles that provide all the “oomph”. With the outer thigh muscles already naturally dispositioned to be stronger contractors, and the Vastus Medialis tending to be weak, improper tracking of the kneecap is, unfortunately, a common outcome.
Six Knee Injury Prevention and Restoration Exercises
Whether a client is a weekend warrior, an overworking joint-abuser, or suffering from some biomechanical malfunctions, these exercises are great for reinforcing and rebuilding knee strength and movement.
The exercises are listed from least advanced to most, so from the most dire knee situation to one that just needs a little extra love.
Exercise 1 – Simple Contraction

For those clients who are just starting to get back into exercise and are struggling with knee mobility and strength.
Sitting with the back against a wall and legs extended in front.
Place a foam roller under the knees.
Be sure that the client is sitting up straight, engaging the abdominal wall to maintain posture. The knees and toes are pointing up towards the ceiling.
One side at a time instruct the client to contract the muscles of the leg to straighten the knee, and then relax.
On the side that the client started with, then instruct them to externally rotate that leg and again begin the contractions.
Depending on the client’s current abilities have them do 8-15 reps of the simple contraction in both positions. Ending the set with a 10-second contraction hold.
Exercise 2 – Supine Leg Lifts
Have the client lie on the ground.
Bend one knee and bring that foot flat on the ground.


The other leg will be lifted to a 90-degree angle to the hip, or as close as they can reach, and then lowered back down.
Tips:
– Be sure the client is keeping their lifting leg as straight as possible
– Instruct them to strongly flex the foot of the lifting leg, it will help keep the leg muscles active and contracted
– During the set, the lifting leg doesn’t return all the way to the ground. Have the client maintain at least an inch between the ground and the working leg during the descent.
Complete 3 sets of 12 reps per side
Progression: Add ankle weights
Exercise 3 – Single Leg Extension in Bridge
Have the client lie on the ground/mat flexing both knees so the feet may lie flat on the ground/mat.

Check that the client’s arms are at their side, and their fingertips can brush the backs of the heels.
With arms at their sides and hands pressing down, instruct the client to lift their hips towards the ceiling while grounding through their heels.
Without the client’s hips shifting down, have them extend one leg, pointing the bottom of the foot towards the ceiling.
Without the client’s hips shifting up or down, they will return the extended leg to the bridge position, and begin on the other side.
The hips maintain the bridge position the entire set
Alternating legs: 8 reps each side, 3 sets
Progression: Add ankle weights
Exercise 4 – Standing Front Leg Lifts



With the client standing, instruct them to point one foot ahead of them with all the body’s weight supported on the other leg
Without allowing the pelvis to tuck or bend through the standing knee, have the client lift the leg toward the ceiling
Gently lower the leg until the toes are on the ground again, maintaining the weight in the standing leg.
Complete 10 reps in 3 sets
Exercise 5 – Moving Warrior II
This yoga pose is especially good for strengthening and bringing awareness to the vastus medialis muscle.



On a yoga mat, from standing, have the client step the left foot back into a runner’s lunge.
The right foot will maintain pointing towards the top of the mat, while the left foot externally rotates until the toes are pointing to the side and the foot is flat on the ground.
The hips and torso rotate open as well, and the arms reach out to the sides.
The right leg is bent, with the knee tracking over right ankle and the heel of the right foot lining with the inside center of the left foot
With the client keeping the right knee line matching with the right shin and second toe line, hold the pose for 5 full inhales and exhales
Then rotate the right foot so both the feet are facing the side of the mat and the client is in a wide straddle. Then rotate the left foot so the toes are pointing toward what was the back of the mat. The right foot maintains its position, flat, and pointing to the side of the mat. Again, hold for 5 full inhales and exhales. This is all 1 rep.
Complete 4 reps in 3 sets
Exercise 6 – Resistance Band Supported Sit Back

With a very heavy resistance looped band, secure one end to something sturdy.
Have the client step within the free end of the band.
The band will rest across the backs of the legs at the very top of the calves, just below the knee joint.
Instruct them to step back until they feel resistance from the band firmly pressing into the legs.
Have the client sit back with the hips, flexing in the knees and allow the band to support the lower legs so they may maintain an almost vertical position in the torso.
By implementing these exercises throughout a client’s regiment, their knees should be strong and sturdy in no time!
References
1. Clark, J. M. (1990). “The organization of collagen fibrils in the superficial zones Of articular cartilage.” J Anat 171: 117-30.
2. Articular cartilage structure, composition and function. Mankin, H.j., V. C. Mow et al. 2000
3. Antipova and Orgel, J. Biol. Chem. 285(10), 7087, March 2010
4. Collagens-structure, function, and biosynthesis. K. Gelse, E. Poschl, T. Aigner Cartilage Research Department of Pathology. University of Erlangen-Nurnberg, Germany 2003
5. University of Michigan, College of Engineering, BME/ME 456 Biomechanics, Cartilage Structure and Function
6. Articular cartilage. Symp Soc Exp Biol 34: 377-95. 1980
7. Mechanics of human joints” Physiology, Pathophysiology, and treatment. Unsworth, A. 1993
8. Basic Orthopaedic Biomechanics, Second Edition, Van C. Mow, Wilson C. Haynes, 1997
9. Material properties and structure-function relationships in the menisci. Colombia University, New York, New York. Fithian DC., Kelly MA, Mow VC. 1990
10. Medical Multimedia Group LLC, Orthopod, 2011, Dr. Randale C. Sechrest.
Beverly Hosford, MA teaches anatomy and body awareness using a skeleton named Andy, balloons, play-doh, ribbons, guided visualizations, and corrective exercises. She is an instructor, author, and a business coach for fitness professionals. Learn how to help your clients sleep better with in Bev's NFPT Sleep Coach Program and dive deeper into anatomy in her NFPT Fundamentals of Anatomy Course.


